A Very Table Genius
How COVID-19 compares to the flu in severity and why it matters
Premise
Tough times call for quality debate about how to respond. Right now that requires understanding epidemiological data. The below table compiles research showing that while influenza is nasty, COVID-19 is much worse. Below it are more details about each component.
Numerical Tentativeness
Perfect numbers don’t exist, especially mid-pandemic. These come from available research, some of it still under peer review. Chances are infection mortality rate data will coalesce with time and larger studies. For now, we all must deal with significant uncertainty. That’s uncomfortable and calls for wearing our big kid pants.
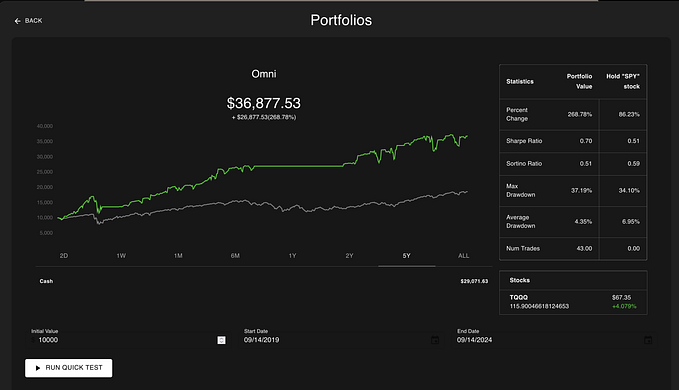
Total U.S. Mortality
Mid-pandemic mortality figures tend to be undercounts. In addition, social distancing reduces transmission and associated deaths, skewing comparisons to other viruses. IHME and machine learning COVID-19 projections for American deaths by early August are 134,500 and 175,500, respectively.
Challenges counting deaths that have already occurred include:
- Post mortem COVID-19 testing for previously untested people, including those with symptoms (especially when tests were/are scarce)
- Cause-of-death accounting methods varying by state or country
- Ascertaining relative cause of death and co-morbidities (e.g., dying FROM or WITH COVID-19)
The seasonal flu average mortality is the mean from the last nine years (estimated 12,000 to 61,000 deaths per year). It includes deaths from multiple influenza strains that circulate seasonally, including H1N1. The 1918 flu death total includes multiple waves.
Case Fatality Rate
This is a ratio of deaths attributed to a virus compared to the number of clinically confirmed cases. Friends don’t let friends confuse it with infection fatality rate (IFR) in “apples to oranges” comparisons. CFR rises where tests are reserved for those at highest risk or severely ill. It is at best a crude indicator of severity. The 1918 flu figures are for the particularly virulent fall wave.
Infection Fatality Rate
This is a ratio showing the average risk of death from infection and is a far better indicator of severity than CFR. A low value would warrant fewer social distancing measures. Thus far more men are dying than women, and risk of death increases with age.
In the table the 0.38% COVID-19 figure is an average of serology tests done globally. The 0.86% comes from recent New York City testing. The seasonal influenza value of 0.04% is the mean of three estimates made by different influenza experts.
Challenges for serology testing used to calculate IFRs for COVID-19 include:
- Test groups not being representative of the larger state or national populations and tending to exclude people too sick or afraid to go out
- False positives significantly skewing data in relatively low-prevalence populations (e.g., Santa Clara, CA)
Average Hospitalization Stay Length
Long hospital stays increase overall disease costs to those suffering as well as the healthcare system. These figures are not as commonly recorded and collected as others in the table. The extra tentative estimates shown here are based on observations by an infectious disease specialist in Hershey, PA. Hospitalization need and stay length both tend to increase with age.
Reproduction Number (R₀)
This indicates the average number of unvaccinated/vulnerable people who will contract a disease from one contagious individual. R₀ is less variable than the Rₑ (effective reproduction rate for a given period of time, also sometimes written Rt). Currently a large majority of the U.S. population is considered immunologically “naïve.” The R₀ value for COVID-19 is the mean of a survey of 16 published estimates. The value for seasonal flu is the median of 47 values from 24 influenza studies.
Complications/Sequelae (note: not included in the table)
It will take years to know the long-term health complications for COVID-19. Those for flu include heart and brain inflammation, muscle damage, and multiple types of organ failure. For COVID-19 doctors have reported cerebrovascular complications (e.g., strokes), brain damage, muscle injuries, and organ damage. One or more of these may occur in 17% of COVID-19 cases.
How Much Worse is COVID-19 than Average Seasonal Flu?
For total mortality it’s clearly spurious to compare a year’s worth of flu deaths to 4 or 5 months of COVID-19 deaths. But even when doing that, ignoring social distancing impacts, and using likely COVID-19 death undercounts, COVID-19 appears twice as deadly. If the current machine learning prediction of 175,400 U.S. deaths is accurate, it would be almost 5 times deadlier after 8 months.
A better comparison incorporates IFR and R₀ to reflect both virulence and contagiousness. The product of the two can indicate overall severity:
IFR x R₀ = :(
For COVID-19 (using a conservatively low estimate for IFR): 0.38 x 2.6 = 0.988
For average seasonal flu: 0.04 x 1.3 = 0.052
0.988 is 19 times bigger than 0.052. So based on current data we could say that COVID-19 appears to be at least 19 times worse than the average seasonal flu. That’s a lot worse, but should be easy to remember.
Short-Term Implications (what the existing data warrants):
- Taking responsibility for our actions, which also have potentially serious consequences for those around us
- Recognizing that being American doesn’t confer innate resistance
- Recognizing the risks essential workers face and both protecting and compensating them accordingly #hazardpay
- Demanding advanced country-style testing to identify people to quarantine and reduce transmission/prevent deaths whenever possible
- Helping coordinate international action to reduce transmission and protect supply chains
- Understanding the need for careful reopening and potential costs of doing so too aggressively (especially without adequate testing)
Thanks for reading and (ideally) sharing and clapping! And if you see any possible errors, please specify. This topic’s too important to get wrong.